The year is 2025, in some city in the interior of São Paulo. doctor Rafael calmly eats his breakfast – a menu specially designed by his “chef” & personal assistant” Alexa, who seeks to improve his health indicators (cholesterol, triglycerides, glucose and others). Your refrigerator is also connected via IoT to your food plan. While sipping coffee, Alexa transmits to him by voice the main information curated exactly for him, as well as the learning path personalized by algorithms that day. Since last year, with the full adoption of Teleradiology, he feels less stressed because he is no longer obliged to spend long hours in hospitals and clinics, going to work at most twice a week. At home, or wherever you are, you use technology that renders in 3D ultrasound images in augmented reality, with perfect accuracy and in real time. Artificial intelligence (AI) software assists you with diagnostics. One of the advances towards precision medicine that Dr. Rafael has been improving is the radiogenomics allowing you to be able to analyze the correlation between cancer characteristics obtained by imaging and gene expression, with better metrics for more accurate diagnoses; organically, he has been diversifying new skills and seeking knowledge in genetics and population health.
At that exact moment, Dr. Rafael is notified that a lady had arrived early at the hospital with chest pain, elevated D-Dimer, history of lupus anticoagulant, and DVT in the left femoral vein. Her clinical data had already been compiled and analyzed by cloud AI and the probability of the patient having a pulmonary embolism (PE) was considered high. The algorithm itself recommended that a computed tomography angiography be performed. It is important to emphasize that it was not the radiologist who requested the CTA, but the machine learning algorithm based on a mountain of data and documents, which it read and interpreted instantly and fluidly. The patient underwent the examination and the AI was indeed correct in pointing out the PE. The algorithm also analyzed bone structures, heart and lung parenchyma, pointing out abnormalities and making clinical and radiological recommendations. The examination (and diagnosis) was then forwarded to Dr. Rafael via app, which analyzes him right after he gets up from the table and goes towards his home office.
As we imagine this possible future, the question that arises is: what will be the main role of Dr. Rafael and his fellow radiologists from now on?
In 2025, society as a whole already better understands the impact of the coronavirus that hit the world in 2020 from an evolutionary systemic perspective. Looking at the last 5 years – turbulent and recessive due to the pandemic crisis – it seems obvious our interdependence It is interconnectivity. There is a growing human awareness of how the planet really works and that unbridled economic growth has culminated in increasing social and environmental losses, which have caused collapses, inequality, poverty, disease, loss of trust in institutions, and also led to the pandemics of the 21st century , SARS, MERS, AIDS, influenza and coronavirus.
Five years ahead, people are more prepared for the “black elephants” which are those events that are extremely likely and widely predicted, but generally ignored, and that people tend to consider them as a “black swan” when they happen, as was the case with the COVID-19 pandemic that had already been predicted and that cost millions of lives. With the advancement of AI and Big Data, it is already possible to learn from past pandemics, gathering relevant data and purifying knowledge to create more resilient environments, and better prepare to respond to potential health crises such as new pandemics.

Returning to 2020, we are already starting to feel these “post-normal times”. We already feel that the notion of speed it's been changing. Everything becomes digitized and becomes exponential. Acceleration is accelerating! What used to take years can now be accomplished in days, or even seconds. The rate at which “new” trumps “obsolete” is staggering. An example? The GPU software manufactured by Nvidia, in 2015, needed 25 days to train ResNet-50, an extremely complex algorithm (arguably more complex than most all imaging algorithms); in July 2020 the new GPU allowed this learning to take just a few minutes; if this pace is maintained, in 2025, it will take seconds.
The world is not only moving faster, it is also becoming a “small” place. A small event, in a tiny village, can impact opposite ends of the globe at great speed. Air travel and the constant international movement of goods and services can spread a virus from one village to a global pandemic in a matter of weeks and days. Near-immediate 24-hour news broadcasting and social media can turn insignificant news into a global spectacle in a matter of minutes.
the notion of scale also changes. Global events quickly have community and individual impact. What happens at an international level affects the lives of people across the planet – financial crisis, pandemics, terrorism, climate change, new application development, surveillance and even shortages of medical equipment. We can no longer ignore what happens in some remote corner of the planet, because the impact of these events is quickly being felt around the world.

A volatility characteristic of the VUCA world becomes even more pronounced with the proliferation of simultaneity. Crises are no longer localized – in a given community and in the lives of individuals – but several of them tend to appear at once! Technological advances have allowed us to clearly map the effects of an economic crisis, a political crisis, which occur simultaneously with a public health crisis. In 2018, the Ebola and MERS epidemics occurred simultaneously. Currently, most scientific discoveries and inventions are made simultaneously by several groups of scientists. A single event can trigger a chain of events that leads to the concurrency of all.
In the face of these post-normal times, how can radiologists prepare?
The main weapon or tool to deal with uncertain and complex times is the development of one's ability to navigate them. And for that, the ability to be in constant learning is fundamental. How do you propose astro teller, head of Google's research lab (X Company), the only way to stay stable these days is to be on the move all the time. Using the bicycle metaphor: we are in balance when we are pedaling. What was it Teller called "dynamic stability". And this is exactly what one of the most talked about concepts is about the skills needed to deal with the future: lifelong learning or continuous learning – an important way not only to think about education, but also work in the 21st century. This concept goes far beyond formal education, recognizing that the source of this continuing education is multiple, vast and coming from numerous domains.
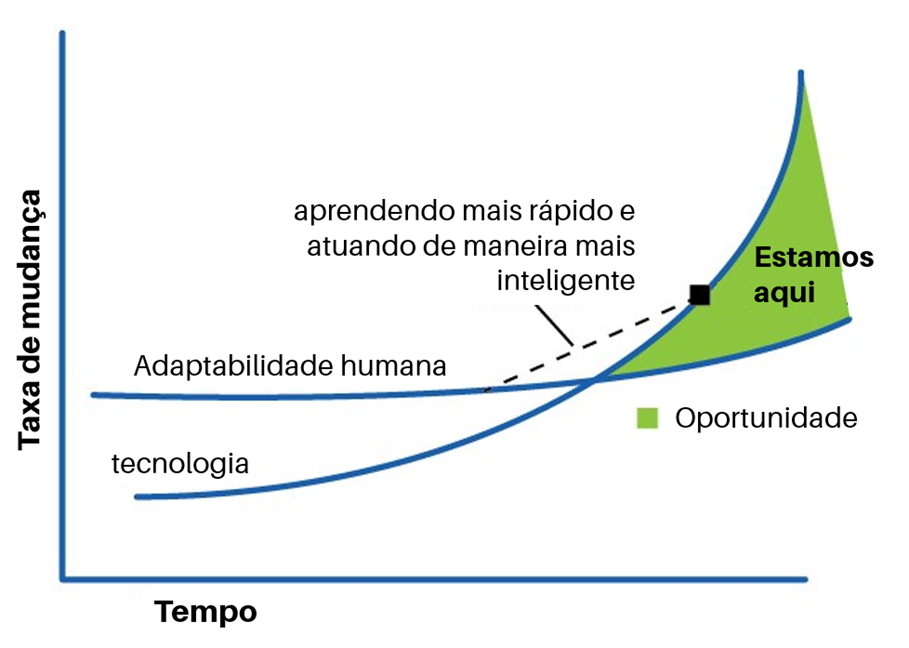
The concept of lifelong learning perfectly applies to the challenges that lie ahead in Radiology for professionals to remain relevant. The dimension of lifewide learning (education that embraces all aspects of life) emphasizes the complementarity between formal, non-formal and informal learning. Learning evolves from accumulating knowledge to working on knowledge flows with a transdisciplinary mindset of human-tech collaboration. It's analogous to learning to master a single instrument versus learning to conduct an orchestra.
doctor Atul Gupta, chief medical officer for Image-Guided Therapy at Philips considers that the Collaboration is the most important capability that radiologists need to be aware of and develop. “Often, other specialties call on us to solve problems that are unique and singular, and this allows me, as an interventional radiologist, to be creative. If I go forward 10 or 15 years, I wouldn't be surprised to see a blurring between specialties, because many of the procedures we do are increasingly overlapping. Who today specializes in critical limb ischemia (CLI), or AAA, or venous disease? Many cardiologists, surgeons and interventional radiologists. I think we're starting to see doctors coming together and learning different specialties. I saw vascular surgeons, cardiologists and radiologists joining the CIRSIS.[…] we also see several specialties coming together. None of us work in a vacuum, so pushing boundaries [silos] to serve the patient is extraordinarily important, not just for clinicians, but for the entire industry. Collaboration leads to the best in innovation.”
With the growth of remote work – as well as Telemedicine and Teleradiology – the ability to collaborate it becomes even more important for physicians to work productively, participatively and collaboratively in virtual teams, generating engagement and trust among their peers or patients.
One of the things that really needs to improve is the quality of diagnostic accuracy, believe doctor Samir S. Shah, who serves as VP of Clinical Operations for Radiology Partners. “We radiologists are human, we make mistakes. […] So, I believe that AI is a great way to verify and benchmark the work of radiologists. It can be an amazing tool without the stigma of current peer review systems, which don't focus on learning.”
Like a self-driving car “driver” or an airplane pilot using autopilot – in this case the AI –, it is as if the radiologist knew your route plan (or flight plan) inside and out, being ready to take over control at any time.
Although radiologists don't know how to build an MRI scanner, they do know how the fundamental concept works. The same applies to AI. “We are not going to know how to make our own algorithm or model, but we have to understand what were the principles that went into it and how it was developed. […] I think it's important for future radiologists to be familiar with many of the concepts that unfortunately are not being taught right now. […] they don't teach us how an AI system works, or what data science is and so on.”, alert doctor Matthew Lungren, director of the Stanford AIMI Center; Assistant Professor of Pediatric Radiology at Stanford University Medical Center.

The problem is, how believe Dr. Nina Kottler, young radiologists are not being prepared for the future of the profession. Dr Nina, who is Vice President of Clinical Operations at Radiology Partners, argues that you need to understand the basics of how algorithms work to be able to speak the language of AI and data and understand potential biases. “Future radiologists will need to provide guidance and advice based on the knowledge generated from these systems. We also need radiologists who can translate clinical cases for AI developers to ensure that the new models that are created add value to our patients and healthcare systems..”
In summary, radiologists today need targeted machine learning training to understand what can go wrong and identify when something goes wrong.
“Radiology is at the forefront of many technological advances in medicine, but radiologists need to adjust their perspectives if they are to remain relevant.”. That was the message given by physician Valerie P. Jackson, president of Radiological Society of North America (RSNA), at the annual meeting in 2019. She urged radiologists to seek to create a more direct connection with the patient. For her, radiologists need to examine more closely the experience of patients and ask themselves how they feel, what they want to know, how they would like to be treated. “It is necessary to create a new culture of interaction with the patient within radiology", she says.
“We will take greater steps in the next decade to play a more integrated role in patient care.” – Jonathan Flug, MD, musculoskeletal radiologist at Mayo Clinic in Phoenix.
Returning to our initial question: what will be the main role of Dr. Rafael and his fellow radiologists from now on?
Global access to more powerful computing, 5G and greater connectivity will further democratize medical knowledge and expertise. This will lead to a future where all physicians (not just radiologists) will develop medical imaging expertise in their daily practice as technology spreads diagnostic imaging expertise – eliminating the need for interpretation and delivery within the domain of a specialty completely separate from the way it happens today.
“In the next decade, it will be the soft skills of radiologists that will make us valuable individuals in healthcare.” believe Arun Krishnaraj, MD, MPH, Professor Radiologist and Chief of the Imaging Division at Virginia University. “It will be our ability to integrate and navigate the vast trove of data across a variety of silos to be at the health nexus that will make us the drivers of decision-making.”, he adds.
Rather than being the radiologist who interprets more and more images and in the quest for a shorter response time, Krishnaraj recommends improving direct communication with patients, enhancing consulting skills with physicians from other areas and modeling collaborations with pathologists. , geneticists and other specialties. “And at any time”, he says, “be willing to embrace any new skill that comes along”.
The radiologists of the future will act as information specialists, contextualizing all the information from different AI systems and using it to consult and communicate with doctors and patients. They will have many more tools to review patient studies, give results and feedbacks snapshots and patients will have better ways to access their images and results.
Faced with so many uncertainties and challenges, we want to invite you to navigate these changing times, together with the most prepared and active professionals in the field of Radiology and Diagnostic Imaging who will be present at the 49th edition of the Brazilian Congress of Radiology and Diagnostic Imaging, which will take place from the 4th to the 11th of October 2020, facilitating the generation of knowledge and scientific and professional connections.
See you there!